Viral comments (38): Biosafety will be sustainable and proportionate or it will not prevail

For almost three decades (the first edition of LBM, Laboratory Biosafety Manual of the World Health Organization, WHO, is from 1983) Biosafety has been implanted, stumbling in some cases, in different countries of different continents. Biosafety grouped and groups together a set of techniques and procedures that seek to control exposure to pathogens, protecting the laboratorial workforce, but also the community that surrounds them, in the face of involuntary or accidental releases. Later, after the attacks of 2001 with anthrax in the United States, public and governments expressed concern about biosecurity, which sought to avoid the availability and use of pathogens, or derivatives, by groups or individuals with intentional purposes. In both cases, a huge amount of technology and money has been poured into devices and systems so that, right now, in the countries of the first world Biosafety and Biocontainment are highly technology-dependent. All research centers on high-risk pathogens in these countries have complex heat ventilation air systems, absolute air filtration, negative pressure cascades between rooms that are maintained 24 hours a day, 365 days a year, liquid and solid waste disposal systems (incineration, alkaline digestion, autoclave), electronic control of access, interlocking doors, showers at the exit of personnel and other measures. And all this shoots up costs dramatically. And maybe it was not that, comrades.
Even small laboratories have high costs; the total construction costs of a 30m2 laboratory and necessary equipment, of Biosafety 3 level (BSL3) in 2009, rose to 400,000 $ (Ssengooba et al., 2015). Consumables and reagents for the first year of operation accounted for an additional 134,655 $. It must be considered that the construction costs for a high containment facility (or BSL3) are around 200-400% higher than those of an BSL2 facility; When operational costs come into play this difference becomes even more pronounced (Abad et al., 2010). Some authors (Heckert et al., 2011) estimate that the annual maintenance budget for high containment laboratories is 10% -15% of the total building cost. And all this drain resources to perhaps more important issues, such as training, qualification and training of the workforce and deep knowledge of good microbiological practices and what you work with.
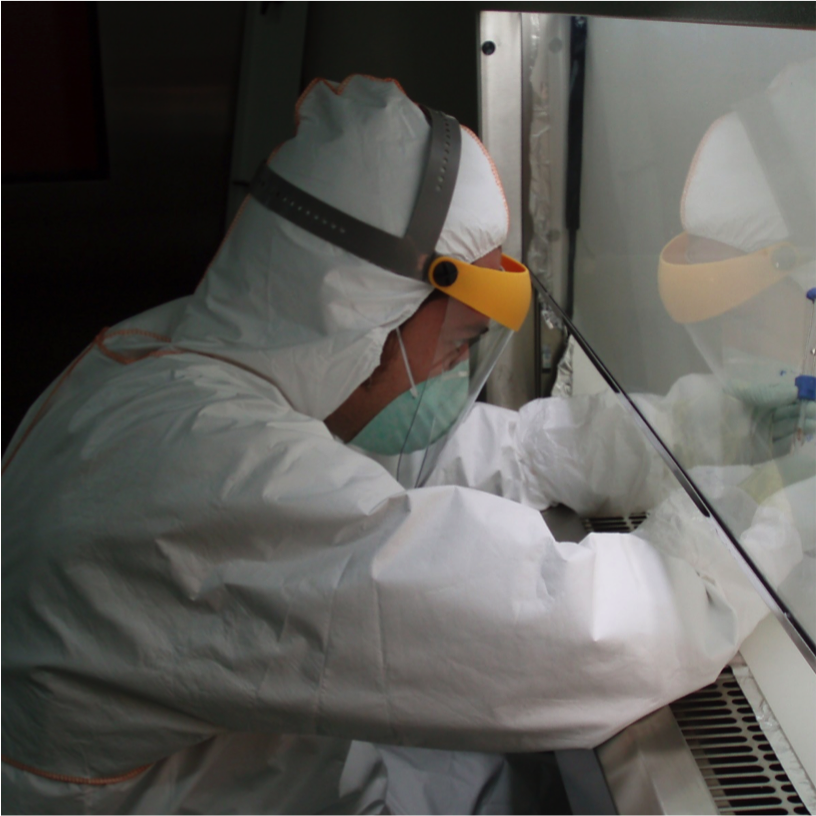
In countries with low or middle incomes, where technology is too expensive, are they doomed not to do research with dangerous pathogens? Do they have fewer rights? Do they have fewer duties? Should your Biosafety be minor because they don’t have the latest technology available? Some of these questions I asked myself (see Abad, 2018) and are also done by others; designing, building and maintaining complex facilities can reduce resources that are already limited by daily laboratory operations, and prevent adequate training and training of personnel (Kojima et al., 2018). Perhaps what we have is to return to some origins in which Biosafety is a function of training and procedural activities that are supported, but not exclusively dependent on the latest technology.
Biosafety must be proportional to the danger that is manipulated and sustainable in the environment where it is handled. Is a high biocontainment facility, biosafety level 3, necessary to handle diagnostic samples of a risk group 3 pathogen? What if we know that the electricity supply is far from being guaranteed? And if we do not know if we will have technical personnel to carry out the repair of the negative pressure system? Is a high-containment facility necessary to work with infected or non-infected arthropod vectors that have no ecological possibility of establishing themselves in the surrounding geographical area?
The categorization established by WHO in groups of microbiological risk, at the time, was associated with certain levels due to its safe handling. However, these biosafety levels, 1, 2, 3 (high containment) and 4 (maximum containment) have been sacralized, perhaps excessively, assuming a linearity, what belongs to RG3 must always be manipulated at a Biosafety level 3, which It is not correct … in many cases.
The risk of handling a pathogen (or samples that may contain it) is multifactorial. It depends on the quantity (volume) and load (infectious titer, concentration), the agent being handled, its infectious dose and pathogenicity, the route of infection and the ease of transmission, the severity of the infection (from benign to mortal), the endemicity of the pathogen (which is country-dependent; Zika is endemic in Brazil but not yet in Catalonia), the susceptibility of the human or animal population that surround activity, the activity we do with the pathogen (diagnosis, spread, infection in animal models, etc.) and the competence or training of laboratory personnel. And we probably are forgetting factors.
Many of the factors that I have just mentioned and that contribute to risk cannot be managed from pure technology and require a risk assessment, which will be area-dependent. We cannot rely biosafety and biocontainment only in technology because we will loose sight of the ecological factor and, more importantly, the human factor. A risk assessment must be applied that puts the activity at the center and that selects the combination of Biosafety elements and practices that best suit a reasoned and reasonably reasonable set or combination of technological elements (biological safety cabinets, specific PPEs or safety solutions from engineering).
Obviously, since the risk assessment will be a dependent area for the same activity, we can have several evaluations that can be all correct. All this will lead to activities that will not be categorized as running in facilities of level 2 or 3 or 4, although incorrectly they also spoke, and are spoken, of facilities 2 plus (+), or 3 +, or 3 enhanced, if not in a continuum of approximations. It sounds a bit anarchic but it will probably better reflect the variability of the activities. It is not the same to work with samples of Chikungunya (RG3, therefore to manipulate in BSL3) for diagnostic purposes, knowing that they have little or no viral load, in a non-endemic zone or with potential vectors (or in an endemic area in the stations without active vectors) than in a facility that produces tens of liters of virus to prepare antigen for a vaccine or that is making an experimental infection in mosquitoes in a non-endemic area where these mosquitoes are native (where the activity should be placed in a BSL3 facility).
We are not inventing anything, on the other hand. Already WHO, the Laboratory Biosafety Manual of 2004 spoke of the need to make local risk assessments. But it was much easier to extrapolate between the microbiological risk groups and the biosafety and biocontainment levels, which are more automatic and require less mental exercise. The result of all this is that the technology has tensed strongly the costs of containment facilities without considering that a local risk assessment, which took into account parameters such as the presence of the pathogen in the area (endemic) could allow an approximation more proportionate and sustainable, and therefore more favorable for human and animal health than tons of engineering. Because, what would be the point of building a maximum containment facility, level 4, to work with the Crimean Congo hemorrhagic fever virus, VFHCC, a RG4 pathogen, if we have infected with VFHCC in the area, and infected ticks roam the same, being an endemic area? This is the case of Turkey; Turkey does not need a BSL4, what it needs is a network of improved BSL2 or BSL3 for rapid diagnosis. This implies an obvious reduction of costs but puts the emphasis on the procedures and the training of the personnel that manipulates these samples.
Another example, diagnostic activities with arthropod borne viruses as West Nile Virus, Chikungunya (Chik) and Zika; the first two are RG3, the third one is RG2. What would mark the “guide” would be to make an equivalence between RG and BSL and therefore the diagnostic samples (sera of horses or birds, to diagnose WNV or mosquitoes captured in the wild to isolate Chik) would be manipulated in BSL3. In Catalonia, a non-endemic area, however, a local risk assessment could indicate that the more than likely low viral load of the samples, and the fact that the sample is, firstly homogenized and inactivated to extract the nucleic acid to further amplification (molecular biology) and that there is no virus culture, would allow carrying out the sample handling under BSL2 conditions.
In summary, before each sample or group of samples it is not necessary to apply a check list depending on what we want to isolate, assuming that it will be in a considerable number of samples and in a high degree … it must be based on the available evidence, and the measurable risks, and in the history of previous samples or origins.
In short, perhaps what needs to be put in the center are the procedures and the personnel, their training, training and competence, which have been perhaps too abandoned while pursuing the holy grail of almost absolute safety through engineering. Because as I pointed out in a previous article, the strength of a chain is based on its weakest link (Callaway, 2012), and on the road of activities with dangerous, potentially lethal pathogens, a Ferrari in hands of a monkey will lead us safely to the disaster, but that a person with a license (trained and qualified) drives us in a small car, it may not be too comfortable, it may not be glamorous, it may not be fast, but it will definitely be safer.
But this, this is another story.
References:
- Abad, F.X. Solanes, D., and Domingo, M. (2010). Reflections on biosafety: do we really know what biosafety, biocontainment, and biosecurity mean? Contributions to Science. 6,1.
- Abad, X. (2018) Biocontainment in Low Income Countries: A Short Discussion
- Medical Safety & Global Health 7:2, DOI: 10.4172/2574-0407/1000140
- Callaway, E. (2012). Biosafety concerns for labs in the developing world. Nature 485, 425.
- Heckert, R.A., Reed, J.C., Gmuender, F.K., Ellis, M., and Tonui, W. (2011). International biosafety and biosecurity challenges: suggestions for developing sustainable capacity in low-resource countries. Applied Biosafety. 16 (4),223-230.
- Kojima K, Makison C, Summermatter K, Bennett A, Heisz M, Blacksell SD, and McKinney M. (2018). Risk-based reboot for global lab biosafety. Science 360 (6386), 260-262.
- Ssengooba, W., Gelderbloem, S.J., Mboowa, G., Wajja, A., Namaganda, C. Musoke, P. et al. (2015). Feasibility of establishing a biosafety level 3 tuberculosis culture laboratory of acceptable quality standards in a resource-limited setting: an experience from Uganda. Health Research Policy and Systems 2015, 13:4