Viral Comments (40): Biosafety through risk assessments. More flexibility, for sure, but more dispersion aswell?
The release of the new Laboratory Biosafety Manual of the World Health Organization (WHO) is imminent. The last edition dates from 2004 and has become one of the reference texts although it does not provide technical information but rather gives advice and organizes how to approach the world of Biosafety through the classification of microorganisms according to their risks and the corresponding levels of Biosafety of the facilities and their requirements.
The new version will be unsettling to many since it supposes a quite radical change; we will move from a prescriptive approach (if-you-want-to-work-with-this-pathogen-you will need-these-measures) to an approximation based on the risk assessments based on evidence (if-work-with-a-given-pathogen-at-a-certain -concentration-to-do-this-technique-with-this-personal-and-facilities-and-the-information-of-the-transmission-of-the-pathogen-is-this-one, the-laboratory-infections-described-are -those, how-to-manage-the-biological-risk-as-a-whole?).
The WHO is targeting a very broad audience that ranges from those responsible for Biosafety in advanced economies such as ours to managers of facilities or hospitals in third world economies where continuous access to personal protective equipment (gloves, masks, etc.) or the programmed maintenance of critical equipment is far to be assured. You can imagine that the Biosafety applied in both places is very different but the fact is that these differences can occur within one state. In some other posts you have read me disapproving of those who talk about Biosafety Level 3 (BSL3) plus or BSL3+ or BSL2+ level facilities but indeed there are BSL3 facilities that are almost BSL4 (like the one I work in) while others are no more than a simply imporved BSL2, or they are modular NBS3. All this stuff is strongly related with economics, too, since the facilities of high or maximum containment are very expensive to build and also to maintain … between 4 and 8 times the equivalent of BSL2 and annual budgets of around 10% of the construction costs ( that is, in 10 years you have spent the equivalent of construction budget). That’s why my advice to those who plan to build a BSL3 in the First World is to ask a question beforehand: have you guaranteed three times the amount of money you’ll need to build the facility? If the answer is yes, go ahead, if it is not, beware!!
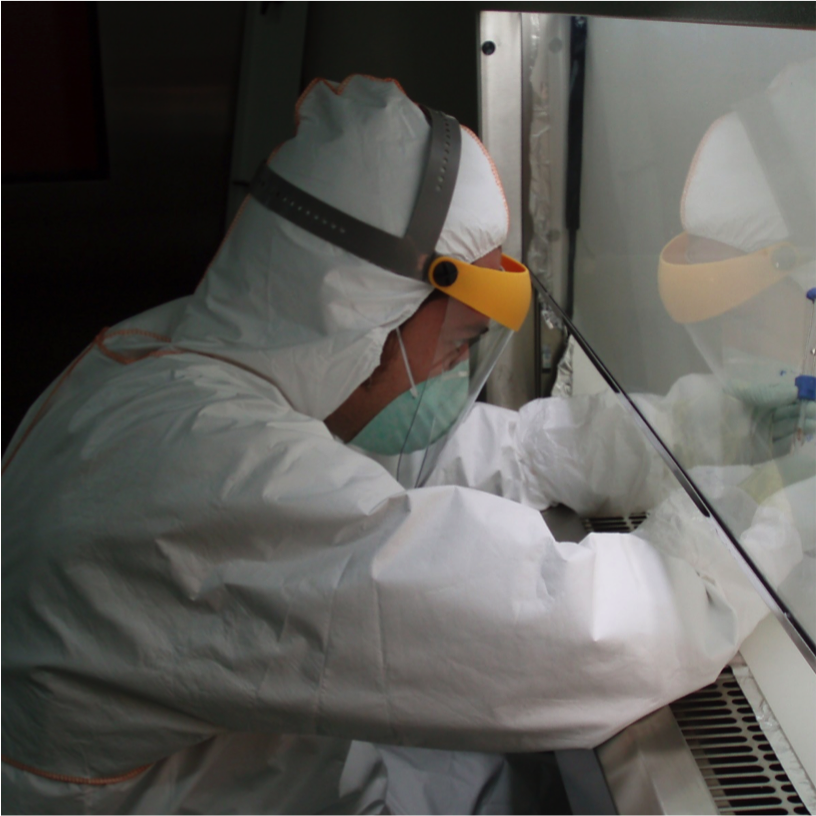
And, maybe, it does not require so much technique (especially if you cannot have it) to handle lethal pathogens. Crimea-Congo, a microbiological risk group 4 virus, which can only be handled at a biosafety level 4 in Catalonia right now, is diagnosed in BSL2 Laboratories in Turkey and the infected are assisted in “conventional” hospitals and there are no reports of laboratorial or nosocomial infections. Similarly, the diagnosis and processing of samples from an Ebola infected patient is not done in complex BSL4 facilities, with negative pressure, positive pressure suits and chemical showers at the sources (Sierra Leone, or Liberia or Congo); a good barrier clothing and a craft cabin with gloves may suffice.
The radical change that WHO will propose will be to stop focusing on a classification of pathogens according to its risks, which brings with it levels of laboratory Biosafety and to consider in each case the adequate containment measures for each pathogen (the source of danger), and the associated processes that we want to do (which will determine the probability of the accident). The risk never depends only on the pathogen if not on the process that is done with it, and each process has its probability of generating damage. And each damage can have varying degrees of severity.
And training, a lot of training. The new WHO manual will greatly reinforce the need for a necessary competence of the staff, and ultimately a good microbiological practice. These are two of the legs of the tripod, together with the risk assessment, with which the WHO wants to sustain Biosafety for at least the next decade.
It is evident that this approach, more based on the evaluation of risk based on evidence (data), is a step towards greater flexibility, or practicability. For the same virus, the measures to be taken may be very different; It is not the same to work with camels infected with MERS coronavirus (high inherent risk) than to make serial dilutions of an inactivated sample … from the same camel, or an ELISA from the sera of these infected animals.
Therefore, what the WHO will ask will be to do risk assessments on a case-by-case basis to determine the minimum requirements for work. As the process becomes more complex or the pathogen becomes more concentrated, etc. additional countermeasures must be implemented.
In any case this Manual is not “regulatory” and has no intention, has never had, to replace or compete with national regulations, although many times these have used the Manual as a basis … therefore, it is likely that this new approach based on risk assessment supported on evidence, and without dogmatisms, ends up getting its space in many countries.
The problem is whether this approach to Biosafety by evidence-based risk assessments will increase the dispersion of approaches. A bit like I’m running this show. And we also do not have so many evidences of transmissibility or not of many pathogens, of its capacity to form aerosols or of its persistence in different environmental conditions, and even less about the emerging ones; many of our data are qualitative or semi-quantitative and would be difficult to consider/accept as “true” evidence.
But this, this is another story.